As we age, our eyes naturally undergo various changes, some of which can lead to common conditions that impact our vision. Among the most prevalent are cataracts and glaucoma. While both can affect vision, they are distinct conditions with varying causes, symptoms, and effects on the eyes.
Understanding the key difference between cataracts and glaucoma is advisable for recognising potential issues and seeking timely professional care. This article aims to clarify these differences, providing you with a comprehensive overview of each condition.
Cataracts: Clouding of the Lens
Cataract refers to the progressive clouding of the eye’s natural lens, a transparent structure behind the iris and pupil. This lens is responsible for focusing light onto the retina, enabling clear vision. Over time, usually as a part of the ageing process, proteins within the lens can break down and clump together, causing it to become opaque.
The formation of a cataract typically occurs slowly, developing over the years. This gradual progression means that symptoms might appear subtle and easily dismissed. Common symptoms include:
- Blurred or hazy vision
- Glare and light sensitivity
- Halos around lights
- Faded or yellowed colours
- Frequent changes in glasses prescription
Risk factors for cataracts include:
- Age: This is the most significant factor, with incidence potentially increasing after the age of 60.
- Genetics: A family history of cataracts can increase your risk.
- Prolonged exposure to ultraviolet (UV) radiation: Unprotected exposure to sunlight is a known contributor.
- Certain medical conditions: Diabetes, for instance, can accelerate cataract development.
- Lifestyle factors: Smoking and excessive alcohol consumption are also linked to a higher risk.
- Eye injuries or inflammation: Trauma or certain eye conditions can also lead to cataracts.
The progression of cataract development varies among individuals. It can range from early, mild clouding that causes few symptoms to advanced stages where the lens becomes densely opaque, leading to potential vision impairment.
Glaucoma: Damage to the Optic Nerve
In contrast to cataract, glaucoma is an eye condition that damages the optic nerve, the critical bundle of nerve fibres that transmits visual information from the retina to the brain. This damage may lead to progressive, irreversible vision loss, often starting with peripheral vision. The most common cause of optic nerve damage in glaucoma is increased pressure inside the eye, known as intraocular pressure (IOP). However, some individuals can develop glaucoma even with normal IOP, a condition referred to as normal-tension glaucoma.
One of the most concerning aspects of glaucoma is its insidious nature in the early stages. Often, there are no noticeable symptoms in the beginning. This is why glaucoma is often referred to as the “silent thief of sight.” As the condition progresses, patients may begin to notice:
- Gradual loss of peripheral (side) vision
- Tunnel vision
- Halos around lights (less common than with cataracts, and usually associated with acute angle-closure glaucoma attacks)
Risk factors for glaucoma include:
- Age: The risk increases with age, particularly after the age of 60.
- Family history: Having a close relative with glaucoma increases your susceptibility.
- High intraocular pressure (IOP): While not everyone with high IOP develops glaucoma, it is the primary risk factor.
- Ethnicity: Certain ethnic groups have a higher predisposition to specific types of glaucoma.
- Certain medical conditions: Diabetes, heart disease, and high blood pressure can increase the risk.
- Long-term use of certain medications: Steroid medications, for example, can raise IOP.
The progression of glaucoma is typically slow, but the vision loss is irreversible once optic nerve damage occurs. This makes early detection and continuous management essential.
Key Differences in Symptoms and Progression
Understanding the differences between cataracts and glaucoma in terms of their symptoms and progression is vital for both patients and eye care professionals.
| Feature | Cataracts | Glaucoma |
| Affected Structure | The eye’s natural lens (becomes cloudy) | The optic nerve (becomes damaged) |
| Vision Impact | Primarily causes blurred, hazy vision, glare, and faded colours across the entire field of vision. | Primarily causes progressive loss of peripheral (side) vision, leading to tunnel vision. Central vision is usually preserved until late stages. |
| Symptom Onset | Gradual, often perceived as a general dullness of sight. | Often asymptomatic in early stages; vision loss is typically subtle and goes unnoticed until significant damage occurs. |
| Reversibility of Vision Loss | Generally reversible with successful cataract eye surgery, as the clouded lens is removed. | Vision loss is irreversible, as the optic nerve damage is permanent. Treatment aims to prevent further loss. |
| Common Patient Complaint | “Everything looks hazy,” “I see glare from lights,” “Colours aren’t as bright.” | “I keep bumping into things on my sides,” or often, no complaint until significant damage. |
| Primary Cause | Protein clumping/discolouration of the lens. | Often elevated intraocular pressure damaging the optic nerve. |
The main distinction lies in what each condition affects. Cataracts affect the clarity of light entering the eye, similar to a dirty camera lens. Glaucoma, on the other hand, affects the cable (optic nerve) that transmits the image to the brain. This means that while a cataract might make everything look dim or yellow, glaucoma can result in missing parts of your vision, especially at the edges, without the central vision being immediately affected.

Diagnostic Methods and Examinations
Given their distinct natures, the diagnostic methods for cataracts vs glaucoma also differ, although both typically begin with a comprehensive eye examination. It is why regular eye examinations in Singapore are recommended.
For cataracts, diagnosis primarily involves:
- Visual Acuity Test: This measures how sharply you see at various distances, often showing decreased clarity with a cataract.
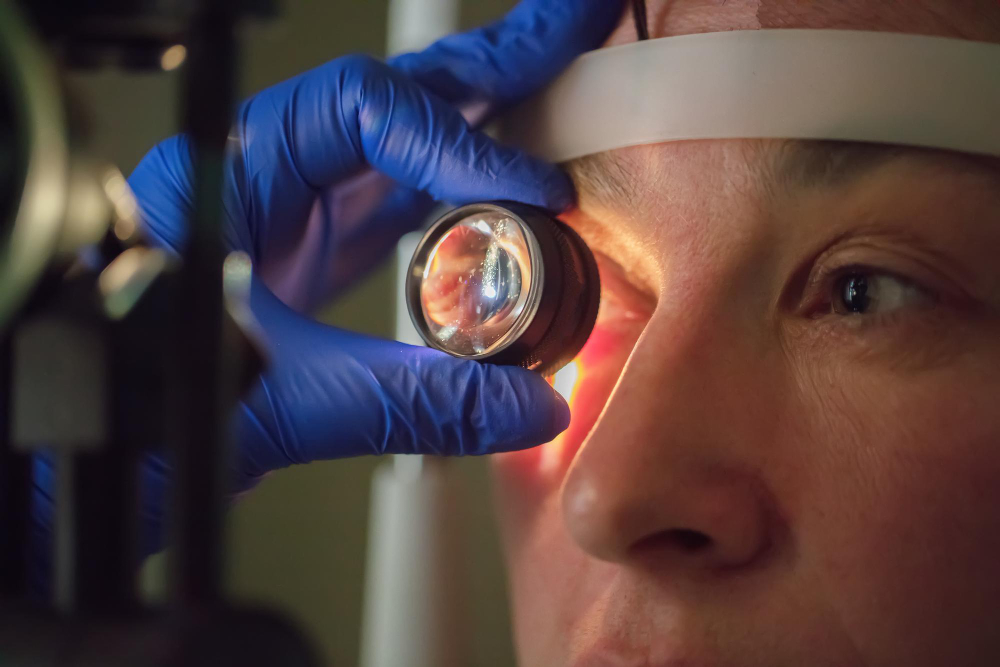
- Slit-Lamp Examination: Using a specialised microscope, an ophthalmologist can observe the detailed structures of your eye, including the lens, to directly visualise and assess the type, size, and density of the lens clouding.
- Dilated Eye Exam: Eye drops are used to widen your pupil, allowing a more thorough view of the lens and the back of your eye.
For glaucoma, diagnosis involves:
- Tonometry: This measures your intraocular pressure (IOP). While high IOP is a major risk factor, it’s not the sole diagnostic criterion. This can be done via various methods, including the ‘air puff’ test or applanation tonometry, which involves gentle contact with the eye.
- Visual Field Test (Perimetry): This measures your peripheral vision and helps detect blind spots caused by optic nerve damage.
- Optic Nerve Examination: An ophthalmologist will carefully inspect your optic nerve for signs of damage, such as cupping (an indentation in the optic nerve head). This can be done using an ophthalmoscope or advanced imaging techniques like Optical Coherence Tomography (OCT).
- Pachymetry: This measures corneal thickness, as thinner corneas can sometimes give a falsely low IOP reading.
- Gonioscopy: This examines the angle where the iris and cornea meet, crucial for classifying the type of glaucoma.
Treatment Options and Management
The treatment approaches for cataracts vs glaucoma are fundamentally different. For cataracts, the definitive treatment is surgical. In the early stages, managing symptoms with an updated spectacle prescription might suffice.
However, once a cataract progresses to the point where it affects daily activities, the doctor may recommend surgery. This procedure involves removing the clouded natural lens and replacing it with a clear, artificial intraocular lens (IOL). Modern IOLs can help correct distance, near, or intermediate vision, or a combination of these, depending on the patient’s needs and lifestyle.
For glaucoma, the primary goal of treatment is to lower intraocular pressure to minimise further damage to the optic nerve. Vision loss from glaucoma is irreversible, so management focuses on preserving existing sight. Treatment options include:
- Eye drops: These are the most common initial treatment, working by reducing fluid production in the eye or increasing fluid outflow.
- Laser procedures: Selective Laser Trabeculoplasty (SLT) or Laser Iridotomy (LPI) can help improve fluid drainage from the eye.
- Surgery: Procedures like trabeculectomy or the insertion of drainage devices are reserved for cases where eye drops and laser treatments are insufficient to control IOP.
It is essential to understand that cataract surgery is a curative procedure for cataracts, replacing the affected lens. A glaucoma treatment in Singapore, conversely, is a lifelong management process aimed at controlling the condition’s progression and preserving remaining vision.
The Potential for Coexistence and Importance of Regular Check-ups
It is entirely possible for a person to have both a cataract and glaucoma simultaneously. In such cases, managing both conditions becomes part of a comprehensive eye care plan. Sometimes, an eye surgery itself can even have a positive effect on IOP for some glaucoma patients, but it does not cure glaucoma.
This potential for coexistence highlights the necessity of routine, comprehensive eye checks for everyone, especially those with risk factors. An eye specialist, such as a cataract specialist or an ophthalmologist, can conduct evaluations that include assessments for both conditions. This approach ensures that any changes in vision or eye discomfort are accurately identified and appropriately managed.
If you notice any changes in your vision, it is advisable to consult with an eye care professional. Early detection and intervention are the most helpful tools against significant vision loss from both cataracts and glaucoma. At EyeWise Vision, our team provides comprehensive eye care, including detailed assessments for both conditions, guiding you towards clear vision and sustained eye health.