Glaucoma Surgery Singapore – Trusted Treatment by a Glaucoma Specialist
Glaucoma is a serious eye condition where elevated intraocular pressure can damage the optic nerve, leading to irreversible vision loss. At EyeWise Vision Clinic in Singapore, our dedicated glaucoma specialist offers comprehensive glaucoma treatment. Whether you require conventional glaucoma surgery or advanced glaucoma laser surgery, our expert team tailors interventions to your unique needs.
What is Glaucoma?
Glaucoma is characterized by increased eye pressure, which can compromise the optic nerve through disrupted blood flow or direct mechanical damage. Often, early-stage glaucoma shows no noticeable symptoms, making regular screening essential. At our clinic, a skilled glaucoma doctor in Singapore evaluates risk factors, ensuring early detection and prompt treatment.
Types of Glaucoma
Understanding the different types of glaucoma is crucial for managing visual health. Here are the types you should be aware of:
| Type of Glaucoma | Description |
| Primary Open-angle | The most common type where the eye’s drainage system is open but not working properly, causing fluid build-up and pressure. This type often has no symptoms until significant vision loss occurs. Regular eye exams are crucial. |
| Primary Angle-closure | This type involves a sudden closure of the space between the iris and cornea, blocking fluid drainage and quickly raising eye pressure. It’s an emergency that can lead to rapid vision loss if not treated immediately. |
| Normal-tension | Here, the optic nerve gets damaged even though the eye pressure is normal. It might be linked to other health issues like poor blood circulation or systemic diseases. |
| Secondary Glaucoma | Caused by other health conditions or medications that increase eye pressure, leading to optic nerve damage. Conditions like eye injuries or diabetes are common causes. Treatment often focuses on the underlying cause. |
| Pigmentary Glaucoma | Occurs when tiny pigment particles from the iris block the eye’s fluid drainage system, increasing eye pressure. It’s a form of open-angle glaucoma. |
| Exfoliative Glaucoma | Caused by flaky, dandruff-like material that clogs the eye’s drainage, raising pressure. This type requires regular monitoring and management to control pressure levels. |
| Neovascular Glaucoma | Abnormal blood vessels on the iris block fluid outflow, often associated with diabetes. This type is serious and needs prompt treatment to manage both the diabetes and eye pressure. |
| Uveitic Glaucoma | Results from inflammation in the eye, which can block fluid drainage and increase pressure. Treatment may include managing the inflammation and controlling pressure. |
| Congenital Glaucoma | A rare condition present at birth where the eye’s drainage system hasn’t developed correctly, leading to increased pressure. Early diagnosis and treatment are vital to prevent vision loss. |
Symptoms Of Glaucoma
While early-stage glaucoma often shows no noticeable symptoms, it’s crucial to stay alert to subtle changes in your vision and see a doctor promptly. Here are some key symptoms to take notice of:
Severe Headaches: Severe headaches can have various causes but are also a prominent indicator for certain types of glaucoma, particularly angle-closure glaucoma. These headaches usually arise from increased eye pressure, affecting the eyes and surrounding structures, causing pain around the eye that may extend to the temples or back of the head. Such symptoms are critical for early diagnosis and warrant immediate eye examinations.
Blurred Vision: Blurred vision may signal several eye conditions; however, if it occurs suddenly and alongside symptoms like eye pain, it could point to acute glaucoma. A medical evaluation by a glaucoma eye specialist in Singapore is essential to diagnose and address this condition promptly.
Gradual Loss of Peripheral Vision: A subtle narrowing of your field of vision, especially on the sides, could indicate glaucoma. Often referred to as tunnel vision, this gradual loss of peripheral sight usually goes unnoticed until it becomes more severe, emphasising the importance of regular vision screenings.
Halos Around Lights: Noticing halos or bright circles around lights, especially in the dark, can be a sign of glaucoma. This symptom can complicate tasks like driving at night or moving in low-light environments and should be assessed for potential glaucoma treatment options.
Eye Pain and Redness: Eye pain accompanied by redness may indicate an urgent type of angle-closure glaucoma. These symptoms are serious and require immediate attention from a glaucoma doctor to evaluate the severity and discuss treatment options, which may include glaucoma laser surgery.
Read More
Glaucoma Diagnosis & Pre-Surgery Evaluation Process
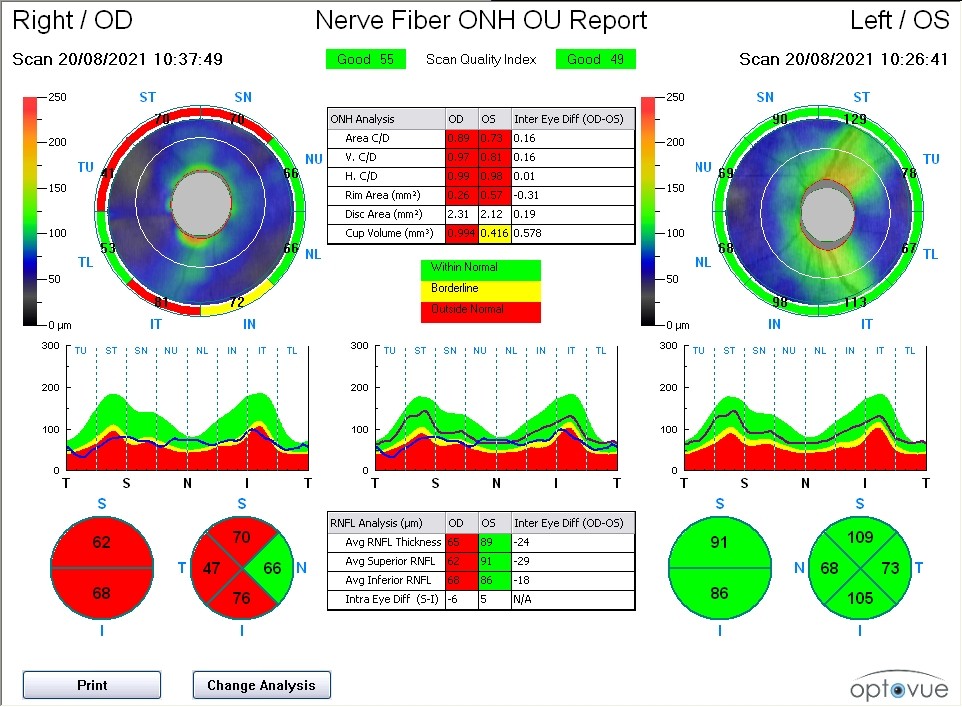
Preparing for glaucoma surgery begins with a comprehensive consultation with your glaucoma specialist in Singapore. In this initial session, your glaucoma doctor will conduct visual field assessments, eye pressure measurements, and corneal thickness evaluations to tailor the surgical plan to your needs.
A visual field assessment is a key test in glaucoma treatment. An automated machine projects light into your field of vision, and you press a button when the light is seen. The system then maps areas of functional and impaired vision, providing crucial information about glaucoma progression and the health of your optic nerve. Typically, this process takes about 5-10 minutes per eye.
At EyeWise Vision Clinic—a trusted glaucoma treatment centre in Singapore—we use the Humphrey Visual Field system, recognized as the gold standard in glaucoma assessment, to collect detailed data for a comprehensive surgical plan.
Following these tests, reviewing your current medications with your glaucoma doctor is essential, as some may interfere with the surgery. Additionally, fasting may be required before the procedure, so please follow the guidelines provided by our healthcare team.
This thorough pre-surgery evaluation ensures that your glaucoma surgery, whether conventional or laser-based, is precisely tailored to achieve the best possible outcome.
Glaucoma Treatment Options: Surgery and Laser Surgery
Managing glaucoma involves various treatment options aimed at controlling eye pressure to prevent vision loss. Here’s a closer look at these options:
1. Glaucoma Eye Drops
The initial treatment for glaucoma typically involves using eye drops to lower eye pressure. Most patients benefit from once or twice-daily dosing, although sometimes two or three different types of eye drops need to be combined to achieve a sufficiently low pressure.
2. Glaucoma Surgery
When eye drops alone do not provide adequate control, patients may require laser or conventional glaucoma surgery. Laser treatment is usually aimed at improving fluid drainage from the eye or reducing fluid production, which helps lower the pressure. Glaucoma surgery is generally performed as a quick, day-case procedure under adequate anaesthesia so that patients experience little discomfort. In some cases, certain chemicals are applied during the procedure to reduce scarring at the surgical site. After surgery or laser treatment, patients are typically prescribed eye drops for several weeks or months to reduce inflammation and prevent infection.
3. Oral/Intravenous Medications
For some patients, intravenous or oral anti-glaucoma medications may be used to lower high eye pressure. However, these medications are not recommended for long-term use due to potential side effects on the body.
About Dr Christopher Khng
Dr Christopher Khng specialises in Complex Cataract and Anterior Segment Reconstruction Surgery, particularly Iris Reconstruction and Surgery for Aniridia. His other areas of expertise include Complex Lens Surgery, New Lens and Phacoemulsification Technologies, Refractive Surgery, Phakic IOLs (the Implantable Collamer Lens, ICL), and small-incision, topical anaesthesia phacoemulsification cataract surgery.
He completed his first two years of medical undergraduate studies at Aberdeen University, Scotland (UK). Due to cost, he completed his medical degree (MBBS) at the National University of Singapore (NUS).
Dr Khng served as Registrar, then Associate Consultant Ophthalmic Surgeon at the Singapore National Eye Centre (SNEC). Following his tenure at SNEC, Dr Khng was a Consultant at The Eye Institute, Tan Tock Seng Hospital, Singapore.
Dr Christopher Khng brings a comprehensive approach to glaucoma care, offering a variety of treatment modalities. His expertise encompasses both medical and surgical management of glaucoma, including trabeculectomy and laser surgery. With a focus on early detection and appropriate treatment plans, Dr Khng aims to manage the progression of glaucoma to help maintain the vision of his patients.
Dr Christopher Khng
MBBS, M.Med (Ophth), FRCS (Edin), AMS (Ophth 2003) Consultant Ophthalmologist
Frequently Asked Questions
Untreated glaucoma can lead to blindness over several years. However, timely treatment can slow down the progression of vision loss or prevent it altogether. It is important to visit a glaucoma doctor in Singapore for an eye screening to detect glaucoma in its early stages and prevent sight loss.
The recovery period after glaucoma surgery varies depending on the extent of the surgery and the severity of the condition. Some people may see improvements in their vision within days to weeks, while others may take several months.
Regular exercise and a balanced diet rich in omega-3 fatty acids can help maintain eye health and potentially prevent glaucoma. Quitting smoking is also highly recommended for maintaining overall eye health and reducing eye pressure. These lifestyle changes should be monitored by a glaucoma specialist.
Performing glaucoma surgery on both eyes at the same time is generally avoided. This approach allows for better monitoring of recovery and treatment outcomes and helps avoid limited vision during the recovery phase.
The success rate of glaucoma surgery generally ranges from 70% to 90%, but individual outcomes can vary based on the type and severity of glaucoma.
Glaucoma surgery aims to prevent further vision loss rather than fully restore lost vision. Once vision is lost to glaucoma, it cannot be fully restored.
After surgery, it is crucial to adhere to prescribed eye drops and attend regular follow-up appointments with your glaucoma doctor to monitor eye pressure and prevent the condition from worsening.
Yes, children can develop glaucoma, although it is rare. Known as paediatric or congenital glaucoma, early diagnosis and treatment are essential for maintaining vision.
Awareness of potential risks is essential for a well-rounded approach to glaucoma surgery. Here are some possible risks and side effects:
- Infection: Bacterial exposure during surgery can lead to infections like corneal ulcers or endophthalmitis, which may cause irreversible vision loss if not treated promptly.
- Scarring: Post-surgery tissue healing can cause scarring that blocks drainage pathways, potentially raising eye pressure and requiring additional treatment.
- Bleeding inside the eye: Surgery can disrupt fragile blood vessels, leading to internal bleeding and possible vision impairment.
- Accelerated cataract formation: Surgical intervention can hasten cataract development, causing blurred vision and necessitating earlier cataract surgery.
Understanding these risks helps ensure patients are well-informed and prepared for their glaucoma surgery.
After glaucoma surgery, avoid strenuous activities and follow your prescribed eye drops to manage inflammation and prevent infection. Attend regular follow-up appointments to monitor your progress, including visual field assessments, eye pressure measurements, and optic nerve evaluations. Report any unusual symptoms, such as persistent redness, pain, or vision changes, to your eye doctor immediately. For comprehensive care, consult a qualified eye specialist at a reputable clinic in Singapore. Also, consider diabetic eye screening, as diabetes can affect glaucoma.



