Cataracts are a prevalent eye condition that affects many people all over the world. In fact, the percentage of elderly patients affected by cataracts is about 78.6%, which also increases as people age. 63.6% of patients are 60 to 64 years while 94.6% of people are those 75 years and older.
A cataract is an eye condition that is characterised by a cloudy area in the lens of your eye that affects your vision. In some cases, you may or may not require surgery to restore clear vision, as eyeglasses and drugs may not be able to improve vision from an already clouded lens. Nonetheless, when this option comes up, there remains a degree of concern regarding the permanence of cataract surgery and whether cataracts can recur after surgery. With this, we address these concerns and shed light on the reality of cataract surgeries and their possible effects on your eyes.
Do Cataracts Recur After Surgery?
The unequivocal answer to whether cataracts can recur after surgery is a resounding no. This is because, during the surgical procedure, the cloudy and opaque lens where the cataract has developed is broken down and entirely extracted from the eye. In its place is an artificial lens known as an intraocular lens (IOL). These specialised lenses are carefully selected to match the patient’s visual needs and provide optimal vision correction.
As a result of the surgery, the cataract ceases to exist within the eye. And as mentioned, it is entirely removed and replaced with a clear, artificial lens, effectively restoring clear vision.
While it is crucial to understand that cataracts do not recur after surgery, the cataract-like symptoms you may be manifesting are due to a secondary cataract or posterior capsular opacification (PCO).
What is a Secondary Cataract?
A secondary cataract or posterior capsular opacification (PCO) is not a recurrence of the initial cataract; instead, it is an entirely different occurrence. During the cataract operation, the new artificial lens is placed within a capsule inside the eye. It is important to note that this artificial lens itself cannot develop a cataract, but the capsule that holds the lens can turn cloudy over time. This is due to epithelial cells left over from your natural lens. When the cells travel due to your body’s natural healing process and accumulate on the surface of your lens capsule, this causes your new lens to be cloudy.
It is worth emphasising that secondary cataracts are typically uncommon. But when they do occur, they can lead to symptoms that mimic those of a primary cataract. This is why some individuals mistakenly inquire whether their cataracts have returned after undergoing surgery.
How Long After The Surgery Do Secondary Cataracts Occur?
Typically, this condition can develop months or even years after the cataract surgery. That’s why it’s essential to meet with your eye doctor regularly and maintain a healthy lifestyle to minimise the risk of secondary cataracts forming in your eyes.
For more information about how to take care of your eyes after your cataract surgery, check out our guide on cataract surgery recovery.
What Are the Symptoms of a Secondary Cataract?
If you’ve undergone cataract surgery, you may be familiar with the symptoms of a cataract. These symptoms are similar to those of a secondary cataract. Keep an eye out for the following signs:
- Blurry vision
- Glares
- Halos
- Difficulty identifying colours, objects, and contrasts
If you experience any of these symptoms, it’s essential to consult your eye doctor promptly for a thorough evaluation.
What Are the Risk Factors for a Secondary Cataract?
Individuals who undergo cataract surgery should be aware of the possibility of developing a secondary cataract. However, the likelihood of experiencing this condition may increase if you have any of the following underlying medical conditions:
- Diabetes-related retinopathy
- Glaucoma
- Retinitis pigmentosa
- A significant degree of myopia (nearsightedness)
- Uveitis
Furthermore, individuals who had complications, such as eye swelling during or shortly after their cataract surgery, may also be at a heightened risk of developing a secondary cataract. It is important to discuss these risk factors with your eye care specialist to ensure appropriate monitoring and management, as needed, to safeguard your vision health.
How Are Secondary Cataracts Diagnosed?
Posterior capsular opacification is typically diagnosed by eye care experts through a thorough eye examination, including the use of a slit lamp exam. This exam involves a special microscope with a bright light attached to it that the eye care specialist utilises to assess the different parts of your eyes.
Additionally, your healthcare specialist will inquire about your medical background and any previous eye surgeries to establish a proper diagnosis.
How Are Secondary Cataracts Treated?
The good news is that treating a secondary cataract is relatively straightforward. The primary procedure employed to address secondary cataracts is known as a YAG Laser Capsulotomy.
YAG Laser Capsulotomy
The YAG Laser Capsulotomy stands as a specialised and precise procedure aimed at eliminating the unwanted cell growth that occurs within the eye’s capsule, responsible for the cloudiness associated with secondary cataracts. Here’s how this procedure unfolds:
- The process commences with topical anaesthetic eyedrops, followed by a YAG laser, which does not cause any external incision. This laser’s highly focused precision allows for controlled access to the cloudy capsule.
- The YAG laser is employed with pinpoint accuracy to vaporise and eliminate the undesirable cell growth within the capsule. This crucial step plays a pivotal role in restoring clear vision.
- As the unwanted cell growth is effectively removed, light can once again travel unimpeded through the now clear capsule, reaching the retina. This renewed ability for normal light transmission results in the restoration of clear vision.
Recovery and Aftercare
Recovery post YAG Laser Capsulotomy is generally rapid, mirroring the brief recuperation period associated with the initial cataract operation. Most patients can swiftly return to their usual activities following their appointment with the eye care specialist. While discomfort is typically minimal, any potential discomfort can generally be effectively managed with readily available over-the-counter pain relief medications, with the advice of a medical healthcare professional, of course.
It’s important to note that, in certain instances, your eye doctor may advise a degree of caution in the hours immediately following the procedure. This may involve avoiding activities such as driving and minimising exposure to overly bright lights during the initial 24 hours post-treatment. Additionally, the use of prescribed eye drops may be recommended to facilitate the healing process and ensure an optimal recovery.
When it comes to treating your cataract, it’s essential to consult a cataract specialist in Singapore for solutions that best suit your condition. That way, not only will you be able to improve your vision but also maintain an optimal quality of life in the future.
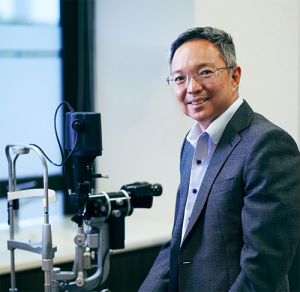
Dr. Christopher Khng, specializes in Complex Cataract and Anterior Segment Reconstruction Surgery, in particular, Iris Reconstruction and surgery for Aniridia. His other areas of expertise include Complex Lens surgery, New Lens and Phacoemulsification technologies, Refractive surgery, Phakic IOLs (the Implantable Collamer Lens, ICL), and small-incision, topical anesthesia phacoemulsification cataract surgery. Dr. Khng is a member of the Singapore Medical Association (SMA), a Fellow of the American Academy of Ophthalmology, the American Society of Cataract and Refractive Surgery (ASCRS), and the European Society of Cataract and Refractive Surgery (ECSRS). He is registered with the Singapore Medical Council (SMC) in Singapore and with the General Medical Council (GMC) for practice in the United Kingdom.

