Cataract Surgery
Cataracts are considered the major cause of blindness and the second most common cause of visual impairment worldwide, with the risk increasing significantly with age. In Singapore, an estimated 78.6% of elderly individuals are affected by cataracts, a number that increases as the population ages.
Furthermore, studies suggest that up to two-thirds of adults with significant, vision-impairing cataracts remain undiagnosed. Given the high prevalence of cataracts, it’s crucial to understand the condition, recognise its symptoms early, and explore options to address it, like cataract eye surgery.
Table of Contents
- What is a Cataract?
- Types of Cataracts
- Causes & Symptoms Of Cataract
- How Does the Doctor Check for Cataracts?
- When to Have Cataract Surgery?
- Cataract Surgery
- Types of Cataract Surgery
- Dr Christopher Khng: Cataract Specialist
- Possible Risks and Side Effects
- Surgery
- Cost of Cataract Surgery in Singapore
- Frequently Asked Questions
What is a Cataract?
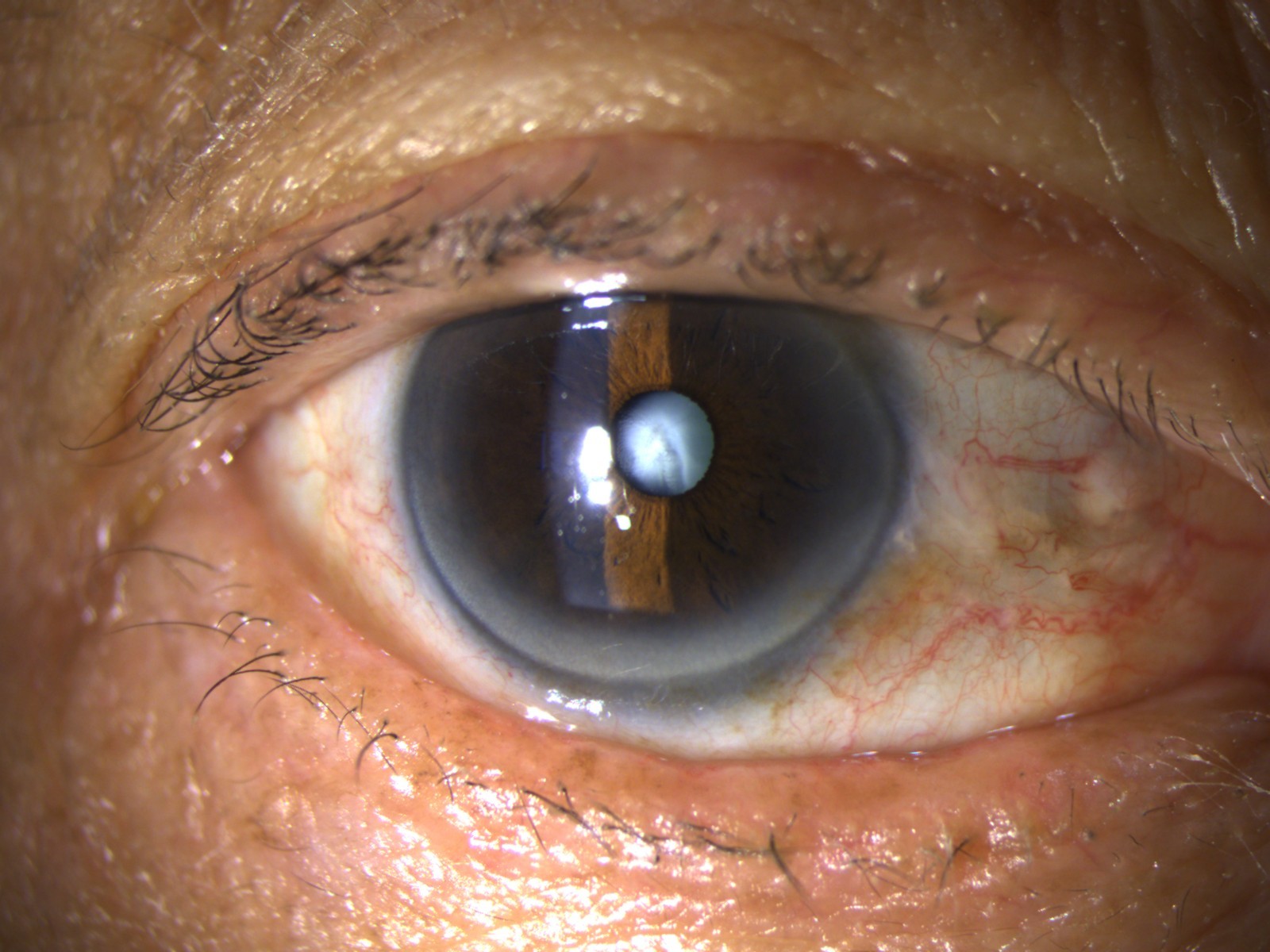
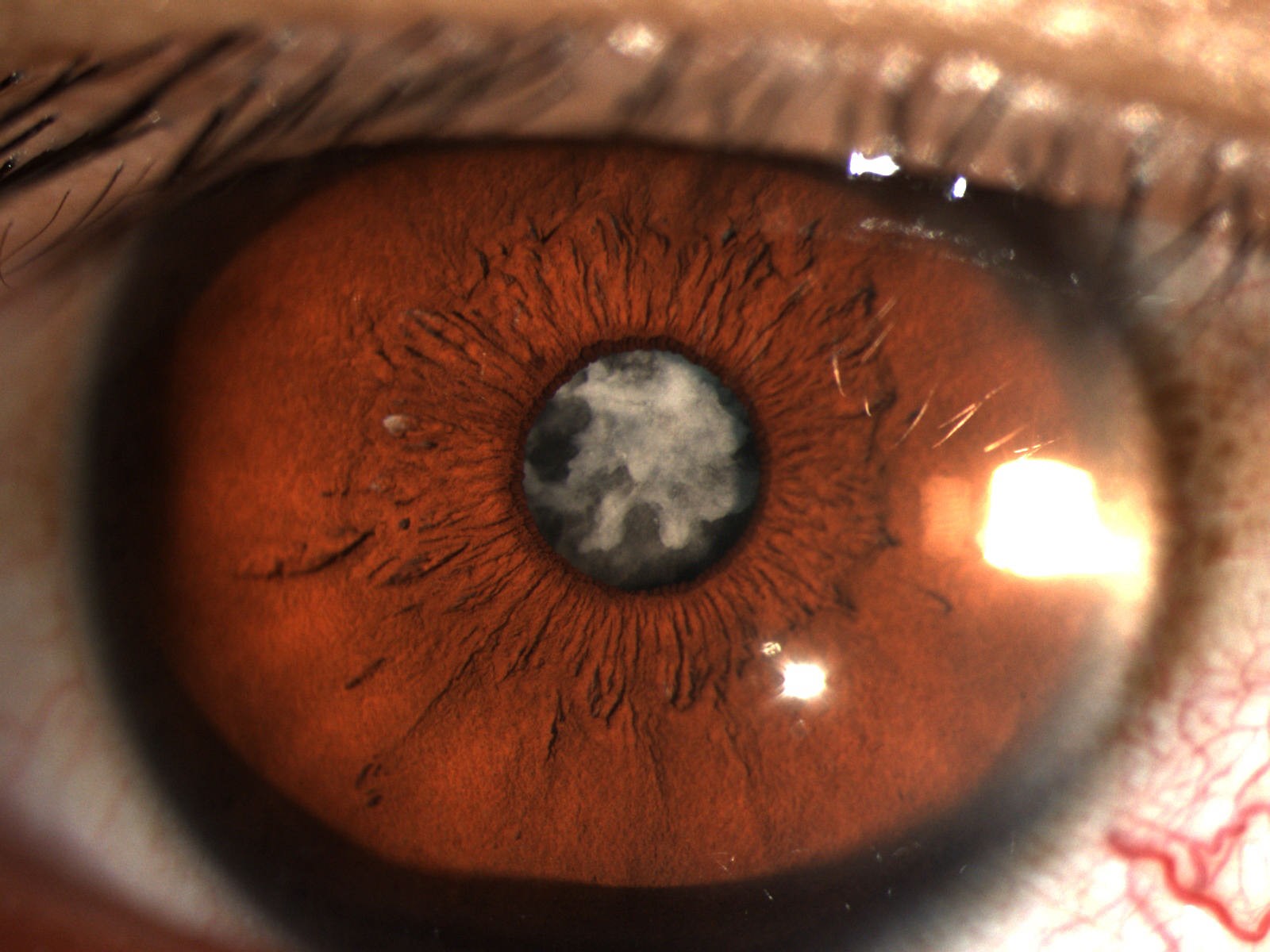
A cataract is a condition that occurs when the natural lens of the eye becomes cloudy, resulting in blurred or impaired vision. This clouding typically starts around the age of 40, as the proteins in the lens begin to break down and clump together. These protein clumps gradually form cloudy patches, which can grow larger and denser over time. If left untreated, cataracts can significantly affect one’s vision and ability to perform daily activities.
Types of Cataracts
The different types of cataracts can impact your vision in various ways.
- Nuclear Cataracts: These develop in the centre (nucleus) of the lens. In the early stages, distant objects will appear blurry, while close-up vision remains relatively clear. Some individuals might even experience a temporary improvement in reading vision. However, as the cataract progresses, the lens can take on a yellow or brown tint, making it harder to distinguish colours.
- Cortical Cataracts: These form around the edges of the lens cortex. They typically begin as white, wedge-shaped streaks or spots that gradually extend toward the centre of the lens. As the opacities develop, they interfere with light passing through the lens, leading to increased visual disturbances.
- Posterior Subcapsular Cataracts : These happen at the back of the lens, directly in the path of incoming light. They often begin as a small, opaque area and can progress rapidly. This type of cataract commonly affects reading vision, causes sensitivity to bright light, and may produce glare or halos around lights, especially noticeable at night.
Causes of Cataract
Symptoms of Cataract
While ageing is the main cause of cataracts, other factors can also contribute to their development. This includes:
- Prolonged exposure to ultraviolet (UV) light,
- Long-term use of medications like corticosteroids,
- Medical conditions such as diabetes
- Eye injuries
- Some cataracts can also be present at birth.
One of the earliest signs of a cataract is blurred or cloudy vision. As the condition progresses, individuals may also experience:
- Frequent changes in prescription glasses due to increasing short-sightedness
- Colours appearing faded or less vibrant
- Sensitivity to bright light and glare
- Seeing halos around lights
- Difficulty reading, watching television, or driving at night
How Does the Doctor Check for Cataracts?
Regular eye examinations with a specialist are essential for detecting potential issues early, including the development of cataracts. During a comprehensive check-up, your eye doctor may perform the following tests:
- Prescription Assessment: Different lenses will be placed in front of your eyes to determine your current visual prescription.
- Intraocular Pressure Test: This evaluates the pressure inside your eyes to help identify the risk of glaucoma.
- Cataract Evaluation: Eye drops will be used to dilate your pupils, allowing the specialist to examine the lens and other structures using a slit lamp to check for cataracts and other eye conditions.
When to Have Cataract Surgery?
Surgery is typically recommended when vision loss due to cataract begins to disrupt everyday activities. In some cases, surgery may also be necessary if the cataract obstructs the monitoring or management of other eye conditions like diabetic retinopathy or age-related macular degeneration (AMD).
There is usually no need for immediate surgery. It’s important to have a thorough discussion with your eye doctor to weigh the risks and benefits and determine the most appropriate timing based on your specific needs and lifestyle. If cataracts are present in both eyes, the procedures are typically done separately, one eye at a time, with the second surgery scheduled a few weeks later, usually about a month apart.
Cataract Surgery
Cataract surgery involves removing the cloudy lens from the eye and replacing it with an artificial lens, also known as an intraocular lens (IOL). This type of surgery is usually performed on an outpatient basis, which means you don’t have to stay in the hospital after the operation.
Types of Cataract Surgery
Micro-Incision Phacoemulsification
This modern technique utilises ultrasound energy to break up (emulsify) the cataract, enabling its removal through an incision in the eye. The cloudy natural lens is then extracted and replaced with a synthetic intraocular lens (IOL) inserted through the same incision. A special liquid sealant is used to close the incision, minimising the risk of post-operative complications.Extracapsular Cataract Extraction (ECCE)
This approach involves removing the entire natural lens through a larger incision, typically around 10mm. The incision is then closed with sutures or stitches. ECCE is typically performed for more advanced cataracts and lasts about 30 minutes. Due to the size of the incision, this procedure carries a higher risk of complications and requires a longer recovery time.Dr Christopher Khng: Cataract Specialist
- Specialises in:
- Complex Cataract and Anterior Segment Reconstruction Surgery.
- Iris Reconstruction and Surgery for Aniridia
- Complex Lens surgery
- New Lens and Phacoemulsification Technologies
- Refractive surgery, including Phakic IOLs (Implantable Collamer Lens, ICL)
- Small-incision, topical anaesthesia phacoemulsification cataract surgery
- Education:
- Initial medical studies at Aberdeen University, Scotland
- Completed MBBS at the National University of Singapore (NUS)
- Career:
- Served as Registrar, then Associate Consultant Ophthalmic Surgeon at Singapore National Eye Centre (SNEC)
- Consultant at The Eye Institute, Tan Tock Seng Hospital, Singapore
- Surgical Expertise:
- Proficient in repairing complicated cataract cases with minimal visual compromise
- Utilises specialised surgical techniques and implant devices, including:
- Standard and modified capsular tension rings.
- Special capsular and iris hooks.
- Specialised sutures.
- Special lens implants can be stitched to the eye’s wall in severely injured eyes.
- What Else You Need to Know About Dr Christopher Khng:
- Trained internationally in complex cataract surgery
- Often referred for complex and advanced cataract surgery cases
- Experience as a visiting consultant focusing on complicated cataract cases
Dr Christopher Khng
MBBS, M.Med(Ophth), FRCS(Edin), AMS(Ophth 2003) Consultant Ophthalmologist
Possible Risks and Side Effects
Generally, cataract surgery is considered a low-risk procedure. However, as with any surgical operation, there is still a possibility of complications. Some potential risks associated with cataract eye surgery include:
- Posterior Capsule Rupture and Vitreous Loss: This complication may arise during the capsulotomy phase of cataract surgery, where an opening is made in the lens capsule to access the lens nucleus. If not performed carefully, this step can increase the risk of vitreous loss, which may impair vision and, in more severe cases, lead to retinal detachment.
- Endophthalmitis: This serious eye infection is caused by microorganisms introduced during surgery. The most common pathogen is Staphylococcus epidermidis, which is naturally found on the skin and eyelids.
- Posterior Capsular Opacification (PCO): Also commonly referred to as a secondary cataract, this condition involves the clouding of the thin lens capsule that holds the newly implanted intraocular lens (IOL) in place. This condition can develop months or even years after cataract surgery, resulting in blurred or hazy vision that is similar to the original symptoms of cataracts.
Make sure to reach out to your cataract specialist should you experience any unusual post-operation symptoms, such as changes in vision, discomfort, or pain. Prompt treatment can help ensure a smooth recovery and optimal outcomes.
Surgery
Cataract surgery is generally a brief procedure, lasting 10 to 20 minutes, depending on your condition. However, patients should expect to spend a few hours at the eye clinic to accommodate pre-operative preparations and post-operative monitoring. After the procedure, the cataract specialist will provide detailed post-operative care instructions along with a schedule for follow-up appointments to monitor your recovery.
During Surgery
Regardless of the type of surgery chosen in consultation with your cataract specialist, the overall procedure generally follows a similar sequence:
- Before surgery, your eye specialist will conduct an eye examination to check your overall eye health and determine the most suitable surgical approach. This is also when you’ll discuss options for intraocular lens (IOL) implants.
- Local anaesthesia will then be administered to numb the eye so that you remain comfortable and pain-free during the procedure. You’ll be awake but relaxed throughout.
- The surgeon will then create a small incision in the eye to access the cataract. The size and position of the incision may vary based on the surgical method used.
- Phacoemulsification or extracapsular extraction is then administered to carefully remove the clouded lens.
- If needed, an artificial intraocular lens (IOL) is implanted to replace the natural lens. The type of IOL will have been selected in advance during your consultation.
- Finally, the incision is either self-sealing or closed with tiny sutures, depending on the method used.
The Day of the Surgery
You will typically be advised not to eat or drink anything for at least 12 hours before your cataract surgery.
The procedure is performed on an outpatient basis, allowing you to go home the same day. However, since you may not be able to drive immediately after the surgery, it’s important to arrange for someone to accompany you and drive you home.
After Surgery
After the cataract surgery, you may experience mild discomfort, itching or a gritty sensation. To protect your healing eye, be sure to avoid rubbing or pressing it and use a protective shield, especially while sleeping, as recommended by your eye doctor.
Your post-operation check-ups will typically be conducted a day or two after the surgery, the following week, and then after a month to monitor the recovery process.
Most discomfort subsides within a few days, and complete healing typically occurs within 6 to 8 weeks. Your doctor will advise when your vision is stable enough for a new glasses prescription, usually between 1 to 3 months after surgery.
Post-Op Guidelines
To optimise your recovery after the cataract surgery, it’s important to follow your treatment plan and observe these recovery guidelines:
- First 12 Hours
- Avoid prolonged activities that strain your eyes, such as reading, using digital screens, or watching television.
- First 24 Hours
- Do not drive or operate heavy machinery.
- First Week
- Wear an eye shield while sleeping to protect your eyes from accidental contact.
- Avoid travel, especially by air, as pressure changes may affect healing.
- First Two Weeks
- Prevent water from entering your eyes while showering.
- Avoid eye makeup and cosmetic products near the eyes.
- Refrain from cooking or spending time in dusty or smoky environments, which may cause irritation.
- Try to stay indoors as much as possible. If you need to go out, wear protective glasses to shield your eyes from light, dust, and debris.
- First Month
- Avoid contact sports, heavy lifting, swimming, and activities that involve heat or steam, such as hot yoga, hot tubs, saunas, or steam rooms.
- While exercising, make sure to prevent sweat from entering your eyes.
Costs
In Singapore, the average cost of cataract surgery ranges from approximately S$9,000 to S$12,000 per eye. The total cost could vary depending on the complexity of your condition, how advanced the equipment is, and the specialist’s experience and seniority. It will also depend on whether the treatment is done in a private clinic or a public hospital.
It’s worth noting that surgery on one eye is not simply half the cost of operating on both eyes. This is due to fixed expenses such as surgical consumables and operating theatre fees, which are incurred regardless of the number of eyes treated.
Most eye care clinics in Singapore offer customised cost estimates based on your eye condition and specific visual needs. These personalised quotes can help you plan financially and make informed decisions about your options.
Which Surgeon or Eye Centre to Choose?
Selecting the right cataract specialist is a crucial step in ensuring optimal treatment outcomes and a smooth recovery. When researching for the right clinics in Singapore, consider the following key factors:
- Credentials and years of experience
- Fully equipped to handle surgical treatment
- Positive patient reviews
- Transparent pricing and care options
It’s important to remember that working with a trusted cataract specialist and a well-established eye centre can give you confidence and peace of mind throughout your treatment and recovery.
Frequently Asked Questions
No. This was true for older surgical methods, but modern micro-incision cataract surgery can remove the lens at any stage. In fact, earlier surgery is often easier and safer before the cataract becomes too dense.
Typically, surgery is done one eye at a time, with a recovery gap of about two weeks. However, simultaneous bilateral cataract surgery may be considered in special cases, based on the patient’s condition and the surgeon’s judgment.
You should consider surgery if cataracts begin affecting your:
- Daily activities like reading, driving, or recognizing faces
- Night vision or sensitivity to light
- Work performance or overall quality of life
- Ability to manage other eye conditions
No. Cataracts are caused by age-related changes in the eye’s lens and will not reverse naturally. The only effective treatment is surgical removal of the cloudy lens and replacement with an artificial one.
Cataract surgery is generally safe, but like all procedures, it carries risks. Complication rates range from 0.5% to 5%, depending on eye condition and surgical complexity.
Possible complications include:
- Posterior capsular opacification (after-cataract)
- Infection (rare)
- Retinal detachment
- Temporary swelling or increased eye pressure
- Lens fragments requiring additional treatment
Most complications are treatable with early medical attention.
Yes. In Singapore:
- Medisave can be used to cover a portion of the cost, subject to withdrawal limits
- Private insurance coverage varies, so it’s important to check with your insurer
Patients are advised to confirm coverage, co-pays, and claim limits before scheduling surgery.
Your original cataract will not return. However, some patients may develop a condition called posterior capsule opacification (PCO) months or years after surgery. PCO causes cloudy vision but is easily treatable with a YAG laser procedure.
Many patients notice vision improvement within a few days, but full clarity may take 1–2 weeks as the eye heals. Individual recovery timelines vary, and follow-up care is important.
Not always. Depending on the type of intraocular lens (IOL) used, many patients experience reduced dependence on glasses. However, reading glasses may still be helpful for some tasks.
You can usually return to light daily activities within a few days, but should avoid:
- Strenuous exercise
- Bending over
- Swimming or rubbing your eyes
Follow your surgeon’s guidance for a personalised recovery plan.